.webp)
A Doctor In Full
Dr. Kheriaty encourages more de-professionalization and de-centralization in medicine.
While pondering their early years in medicine, some doctors, reading Dr. Aaron Kheriaty’s thoughtful and entertaining memoir of being a physician, Making the Cut, will probably think meanly of themselves. I did. Right from the start, while still a student, Dr. Kheriaty demonstrated the proper disposition for a physician. He loved medicine; he was awed by its significance; he was humble; he liked talking with patients; he had a natural bedside manner. In my case, it’s not that I had poor bedside manner so much as I had no bedside manner. I didn’t do bedside manner. Nor, as a young anesthesiologist in training, did I expect to. Once, during my residency, a middle-aged patient informed me of my deficit. I snapped back, “You shouldn’t expect good bedside manner from your anesthesiologist. Just be grateful that you woke up.” To paraphrase Willy Loman, I was not liked, let alone well-liked, by patients.
I changed over the years, but Dr. Kheriaty wisely explains how medicine can accommodate all sorts of odd personalities; even if I had not changed, I would have found my place. Not surprisingly, given his strengths, he pursued a career in psychiatry, where his career flourished at a California university until the pandemic, when he challenged the university’s vaccine mandate policy in federal court and was subsequently fired. Government efforts to censor the medical field through social media control led him to become a plaintiff in the Missouri vs. Biden case, in which the judge decided that the Biden administration had, in fact, violated physicians’ First Amendment rights. Besides having a good bedside manner, Dr. Kheriaty has courage and backbone.
His book opens with the enthusiasm of a young person learning how to practice medicine — enthusiasm gradually tempered by reality. The hours in medicine are long. The smells are bad — he opens the first chapter with a story of having to manually disimpact a morbidly obese patient suffering from constipation. The hierarchy among physicians, stretching from the lowest medical student to the highest attending physician, can sometimes border on the ridiculous. In nineteenth-century Russia, the status of the serf was such that a noble could beat him without suffering legal consequences. Dr. Kheriaty describes a similar experience during his early years in a teaching hospital, where medical students, already emasculated by the shortness of their white coats, can be berated, ordered about, and humiliated by attending physicians, with no right to defend themselves.
Dr. Kheriaty is at his most interesting when he uses those everyday training experiences as a springboard to wax philosophical. In one example, he humorously describes how doctors approach the sensitive subject of sex by engaging in what he calls “the sterilization of the erotic.” By making sex seem no different from bowel habits or joint mobility, doctors try to put patients at ease so they will be more likely to discuss their concerns. Yet the language doctors use to talk about sex also risks changing the way they think about sex. Phrases such as “safe sex” or “sex life” make sex seem like any other physiological process. Gone is the sense of awe and mystery. At the same time, Dr. Kheriaty admits, medicine’s efforts to erect a completely sterile field around sex are useless. “Love and sex remain forever beyond our impoverished clinical words,” he writes.
This last point resonated with me. While a medical student, I learned how to perform a pelvic exam on a live model provided by the medical school. Along with several other male medical students, I waited anxiously outside the building for my turn. I felt like a sailor on shore leave in a foreign port. When my turn came, the naked woman, whose legs were already up in stirrups as I greeted her, told me in clinical language what to do. While proceeding, I must have looked especially nervous and wan under the bright lights, as she asked me, with my hand inside her pelvis, “Are you okay?” “Yes, absolutely, just trying to palpate the ovarian ligament,” I lied in reply, my heart racing.
As for the sterile operating room, where I spent the next thirty years of my life, unsterilized attitudes toward sex inevitably peeped through—interestingly, all in accordance with another hierarchy. Surgeons got away with spouting sexual jokes because they brought the business. Anesthesiologists enjoyed similar freedom, although they couldn’t crack jokes while the surgeon needed to concentrate. Female nurses were also cut a certain slack, as it was deemed less offensive when they, rather than men, teased about sex. Young male orderlies, however, were cut no slack at all. Around naked bodies, they were viewed as a species of dangerous animal to be kept on a tight leash. Without professional status for cover, and already suspect because of their age and gender, they were denied the right to utter anything remotely lewd in the operating room.
Dr. Kheriaty continues his train of thought with an interesting observation about clinical language more generally. Doctors need to use sterile language to remain objective and maintain a degree of distance from their patients, he says. At the same time, such language removes them from the realities of the illnesses they treat. In an example from my own field, “pain” becomes “nociception,” a word devoid of all human feeling. Because of medicine’s stilted language, the sick person is deprived of meaningful words to express his or her anguish. Conceptualizing disease through an arcane language also leads to over-medicalization and hyper-specialization, which breeds more trouble, Dr. Kheriaty writes.
The key, he says, for doctors, is not to solve the contradiction of clinical language. Doctors cannot solve it. But they should be aware of it and keep it in the back of their minds. The goal is not a doctor who has eliminated the contradiction — that is impossible — but one who at least comprehends it, he suggests.
This is really the book's main theme, which Dr. Kheriaty embellishes through personal observations on a variety of subjects, ranging from pain to caring to death. Regarding death, he jumps from a description of a patient's death inside an intensive care unit to the subject of physician-assisted suicide — two seemingly unrelated phenomena. However, he then ties them together in an interesting way. Each is a declaration — and a presumptuous one at that — that death is under our control, he says. Through technology, we decide when we die. Euthanasia and physician-assisted suicide on one side, the obstinate determination to keep dying people alive on the other, become flip sides of the same coin. Both are examples of medicine’s death-denying tendencies.
Once again, there are limits and contradictions. Death can no more be brought under rationalized medical control than sex can, he suggests. If there is an art of sex, there is also an art of dying, and the art of dying involves more than just a morphine drip. It means getting your affairs in order, making peace with certain people, rectifying past mistakes, and having hard conversations. By keeping dying people alive a little longer inside an intensive care unit, artificially maintained by technology as they lie flat in isolation, medicine “engages in a form of theft,” he writes. It steals a dying person’s opportunities to perform these very human tasks. And the person dies anyhow. The key is not to conquer death — it cannot be conquered — but for physicians to recognize the contradiction, that despite all that they do, they will always fail in the long run, since all people die eventually. Sometimes the best a doctor can do is to let people die well.
Toward the book’s end, Dr. Kheriaty offers some worthwhile prescriptions for improving health care in the U.S. He criticizes medicine’s heavy reliance on “evidence-based medicine,” meaning therapeutic algorithms gleaned from controlled clinical trials. Such medicine is based on statistical averages, which apply to large populations but not to any individual case. Demanding uniformity in care based on “evidence-based medicine” can lead to good care for a large patient population but very bad care for a particular patient, he explains. Nevertheless, “big pharma” pushes the concept, he says, because it benefits, since only the pharmaceutical companies can afford to conduct the large randomized controlled trials that generate evidence-based medicine’s algorithms, and that serve as the basis for licensing its products.
The point is interesting not only in its own right but because of who is making it. Dr. Kheriarty would probably be considered a “conservative.” A generation ago, conservatives usually defended big pharma as one of the crown jewels of corporate America. No longer. In the same vein, Dr. Kheriaty often quotes the social critic Ivan Illich, who, when his book Medical Nemesis was published in 1975, was called a crank, certainly by conservatives. Illich warned against a medical profession conspiring with industry to over-medicalize life, to pathologize normal conditions, to gain control over people, and to create in people a false sense of dependency. Even conservatives now admit there was some truth in what Illich said.
As for health care more generally, Dr. Kheriaty encourages more de-professionalization and de-centralization in medicine. An example of the former would be to label more prescription drugs “over-the-counter,” giving people more control over what they put in their bodies. The latter would include giving people more responsibility for their health in general, not to blame them when they fail, but, on the contrary, because, without doctors constantly pushing the latest technology on them, people sometimes stand a better chance of staying healthy. The individual human body, and not any technology, has always been “the primary agent of health and healing,” Dr. Kheriaty reminds us. I must admit, I try to stay away from doctors and medicines as much as possible, taking, at most, a Tylenol or a Motrin from time to time. It’s not that I distrust doctors and medicine (how can I, having worked in the field so long?), so much as I am wary of what they can accomplish. Yes, they offer benefits, but with every benefit in medicine, there also comes a risk. Indeed, in my own field of anesthesiology, the best way to avoid risk is to do nothing at all. I suppose this makes me a walking contradiction: a physician who prescribes medicine while also being somewhat wary of medicine. But then, as Dr. Kheriaty says, a good doctor recognizes such contradictions and learns to live with them.
Ronald W. Dworkin, M.D. is a fellow at the Institute for Advanced Studies in Culture. His other writing can be found at RonaldWDworkin.com
Pursuit of Happiness

The Rise of Latino America
In The Rise of Latino America, Hernandez & Kotkin argue that Latinos, who are projected to become America’s largest ethnic group, are a dynamic force shaping the nation’s demographic, economic, and cultural future. Far from being a marginalized group defined by oppression, Latinos are integral to America’s story. They drive economic growth, cultural evolution, and workforce vitality. Challenges, however, including poverty, educational disparities, and restrictive policies, threaten their upward mobility. Policymakers who wish to harness Latino potential to ensure national prosperity and resilience should adopt policies that prioritize affordability, safety, and economic opportunity over ideological constraints.

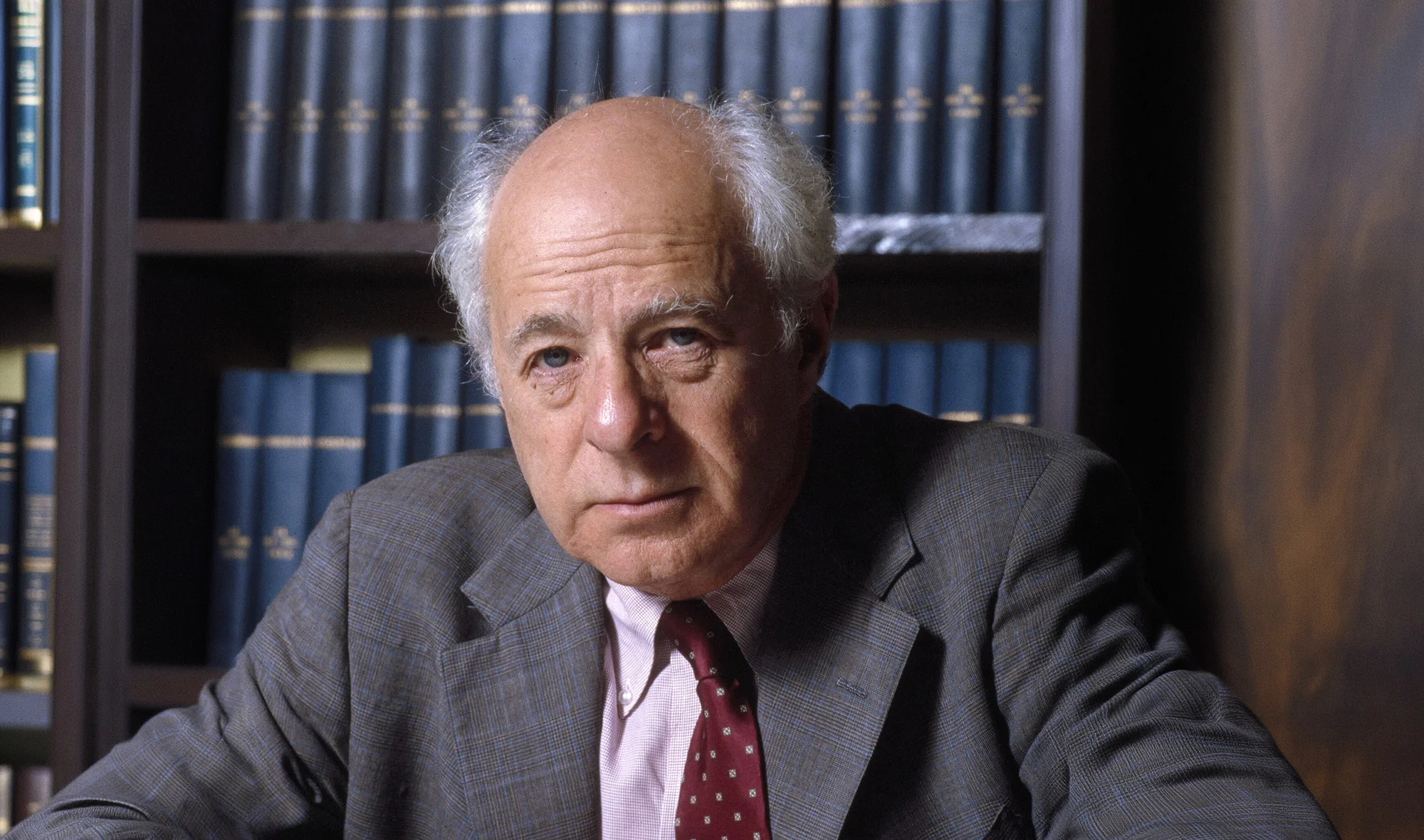
Richard Epstein on Roman Law and Sociobiology
How and why Roman law worked, how it eventually fell apart, and sociobiology as a way to explain the foundations and limits of legal norms.
.jpg)
The False Equivalence of Multicultural Day
Parents have an affirmative obligation to reinforce patriotic values and counter the narratives that are taught in school.
Norman Podhoretz: American Patriot, Faithful Jew, and Indomitable Defender of Civilization
Podhoretz never turned on the promise of America.